Friday, December 22, 2006
Happy Christmas
Kezia's counts were good on Wednesday so she had the cyclophosphamide. However, they booked her in to have Thursday-Sunday cytarabine at the hospital. This is normally administered at home so I had to phone the hospital on Wednesday evening to find out why. Well, it seems it was an oversight and when they went on Thursday they gave her a prescription to have it at home over the weekend.
I expect I won't be blogging over the next two weeks - better things to do like enjoying my family! A happy Christmas and New Year to our readers!
Wednesday, December 20, 2006
UKALL 2003 - Cyclophosphamide and Chemical Warfare
Cyclophosphamide is what is called a pro-drug – that is it doesn't act directly itself but gets changed into something else and this something else does the work.
In the case of Cyclophosphamide it is changed into aldophosphamide in the liver. Most of this is then oxidised by the enzyme aldehyde dehydrogenase (ALDH) into the pretty useless carboxyphosphamide. However, a small amount is converted into the good phosphamaride mustard and the harmful acrolein.
Now phosphamaride mustard is pretty cool stuff! It's one of a group of substances called nitrogen mustards and the first nitrogen mustard, mustine, is on Schedule 1 of the Chemical Weapons Convention!
At the end of the first world war mustard gas was quite widely used by both sides. Although there were only isolated incidents of its use in the second world war, both sides had large stockpiles. In 1943 a U.S. stockpile in Italy was bombed exposing thousands of people. It was noticed that one of its effects was to lower the white blood count – and this led to research into its use as an anti-cancer agent.
My dad was a Gas Identification Officer in the second world war. He worked in a factory producing paint for military aircraft – a protected occupation meaning he didn't get conscripted. After air raids he would have to go out and check that the bombs dropped were not gas bombs. He also went the rounds giving talks to air raid protection people – I remember when I was a child him showing us his sample kit which he would get people to sniff so they would be able to recognise chemical warfare agents. Blimey – if he was found with that stuff today they'd arrest him as a terrorist!
A couple of chemistry diagrams to demonstrate the relationship between cyclophosphamide and mustard gas.
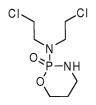
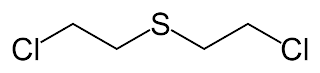
At the top is a cyclophosphamide molecule, below mustard gas. Those two chlorine arms on each side of the nitrogen and sulphur atoms are what make them similar.
And lastly in this little digression – its called mustard because its smell is vaguely similar to edible mustard, not because edible mustard is otherwise faintly related.
The Acrolein is the reason behind all the hydration before and after. It is toxic to the surface of the bladder and can cause hemorraghic cystitis!
Phosphamaride mustard doesn't have much effect in the bone marrow (or liver) as the cells here have high levels of ALDH. Where it does have effect is on leukaemic blood cells where, and they're not quite sure how, it gets to work on the DNA causing cell death.
Usual range of side-effects: nausea, hair-loss, low WBC etc etc as well as the bladder problems mentioned above.
Today, neutrophils and platelets permitting, is Kezia's cyclophosphamide day.
P.S. I have added some dosing information to the post concerning Methotrexate.
Tuesday, December 19, 2006
UKALL 2003 - Dexamethasone 1
As previously mentioned the gluco-corticoid, (a steroid), Dexamethasone has two roles in ALL treatment. The first of these, to combat the side-effect of nausea caused by the anthracyclines. I'll discuss now, and leave its other role until a later date (when I understand it!).
Nausea and vomiting (known as emesis) are controlled in part of the brain known as ... the Vomiting Centre (not often that medical jargon is this straightforward!). The anthracyclines stimulate the production of a chemical called Serotonin (or more correctly 5-HT) in the gut. This Serotonin then binds to and stimulates the vagus nerve which in turn stimulates the spinal cord and the chemo-receptors. There are many types of these receptors sensitive to different chemical compounds and seven of them are sensitive to Serotonin. The one that stimulates the Vomit Centre is known as 5-HT3.
So if we can successfully block, desensitise or turn off the 5-HT3 receptor, then we can stop the nausea – and this is what Dexamethasone (as an anti-emetic) does.
Unfortunately, it has its own side-effects such as increased appetite (Kezia put on weight!), sleeplessness and mood swings.
Kezia definitely suffered from mood swings. I sometimes think it is easier for an older person to rationalise these – I'm grumpy (or as Cass of Cancergiggles calls it – Irritable Bastard Syndrome) but it's due to the medication. Kezia cannot do this and does not understand why she is upset, which must be distressing in itself.
However, there's a downside to the ability for rationalisation that comes with age. Kezia does not understand ALL, cannot imagine her own mortality or the battles still to come. She lives from day to day, oblivious to such feelings – if one day she is down, the next will be happy, not remembering yesterday. For this, we must be grateful.
Monday, December 18, 2006
UKALL 2003 - Daunorubicin and Doxorubicin
Daunorubicin: this is administered during the first Induction phase. It binds to the DNA and intercalates with it i.e. it inserts a molecule of itself in between the DNA molecules. This distorts the DNA, messing with the way it functions and preventing it from replicating.
In the picture above normal DNA is shown on the left and DNA intercalated at three locations (in red) is shown on the right.
Doxorubicin: this is given in the two Delayed Intensification phases (4 and 6). It binds to the DNA and inhibits the enzyme which unwinds the DNA double helix to be read for copying. It stops the enzyme from resealing the double helix thereby stopping replication.
Both drugs are administered by IV drip.
One of the side-effects of both these drugs is feeling sick (nausea) and vomiting. For this the gluco-corticoid (a steroid), Dexamethasone, is given. As well as combatting the side-effect of nausea, Dexamethasone is also used as a first-line treatment drug in later maintenance phases. For this reason, I'll leave its discussion until a later post (as I'm still trying to get my head around how it works!).
Another side-effect of the anthracyclines is hair-loss. In young adults, this can be a major psychological issue (Lucia discusses it in her blog – link on right). However, although it has happened to Kezia, she has not yet developed the self-consciousness for it to be a problem. I think Nanda and I have been more effected – Kezia's hair was so beautiful! However, it will grow back!
Impatience
Friday, December 15, 2006
UKALL 2003 - Delayed Intensifcation 1 and Drugs
This is the fourth phase of treatment and lasts 8 weeks (if all goes well – although as I indicated yesterday, Kezia has had a delay of a week). The phase won't start until your child's neutrophil count (ANC) is >0.75 (x 109/L) and her platelet count is >75
The phase is divided into two parts: reinduction and then reconsolidation. In theory, there is a week's interval between the two but your child won't start the reconsolidation until the ANC and platelet counts are at the levels above.
The pattern of medication is very similar to that of the very first phase.
Let me talk a little bit about some of the medications.
Methotrexate (MTX): This can be administered intrathecally (IT - into the spine) or intravenously (IV - into the veins).
Every so often throughout the treatment your child will have a sample of spinal fluid taken (a lumber puncture). The fluid is analysed to check the leukaemia has not spread to the Central Nervous System (CNS). (If it does, with resultant risks to the brain, your child will be off-protocol and receive radiation therapy). Even when a child does not have CNS disease, methotrexate is administered as a prophylaxis. The lumber puncture and IT MTX are administered under general anaesthetic.
Methotrexate inhibits the production of folic acid which cells need to synthesize new DNA prior to splitting. Therefore the cell cannot split or replicate. It will therefore have a greater toxic effect on fast-splitting cells such as cancer cells but also hair and mouth cells.
During the third and fifth phases, Escalating Capizzi 1 and 2, the Methotrexate is administered into the veins (IV - intravenous). The dose is gradually increased by 50 mg/sq. m. throughout this stage from a starting point of 100 mg/sq. m. but is stopped at signs of toxicity – either low neutrophil counts (neutropenia), severe mucositis (sore/infected mouth) or liver/kidney dysfunction. In the case of a low neutrophil count, when it has recovered your child will restart at 80% of the last dose. In Escalating Capizzi 2 the starting dose is 50 mg/sq. m. below the final level attained in Escalating Capizzi 1 and then increased by 50 mg/sq. m. but again decrease the dose if toxicity occurs. In the case of mucositis the dosing alterations follow different rules.
In Kezia's case she only had two doses of IV methotrexate (week 15 and 19 - 100 mg/sq. m and 80 mg/sq. m) as her neutrophil counts were too low on the other occasions. I was initially concerned about this and consulted J. He reassured me that this was actually a good sign – the methotrexate was doing its job fine without the need for more and higher doses. She will start Escalating Capizzi 2 at 30 mg/sq. m.
I will continue with other drugs in forthcoming posts.
New Links
Thursday, December 14, 2006
Open Source
As promised, I will now go off-topic. The subject for discussion is Open Source software.
First, I need to define this for you (bear with me if you already know what it is). From Wikipedia “Open source describes practices in production and development that promote access to the end product's source materials — typically, their source code”.
The concept of open-source can be applied to more than just computer software, for example it has also been applied to media other than computer programs, such as books, music and photos, e.g., by Creative Commons. It has also been applied in such fields as scientific and medical research (which I may try and blog on in the future).
For a more in depth analysis of the whole open source concept, I'll refer you to Wikipedia's entry.
However, amongst all the myriad advantages two major ones stand out. Firstly, it allows users/developers to build on previous developments to create new products to serve better or differently the community of end-users. Secondly, the end-product is free!
This blog is written on a machine running on an open-source and free operating system, Linux (version OpenSuse 10.1 for the techies). It's available as a commercially available system from Novell. How does Novell make any money from it, if it's also available for free? Basically by providing support contracts for large corporations who cannot afford to have any downtime. Novell also benefits from the hoards of non-Novell developers working on improving the product – they can then incorporate these improvements into their next commercial release. Additionally, if you have the free version, then there are lots of user and developer groups out there to help you.
Another big advantage is that because Linux is free, it is a lot less prone to viruses – the virus writers love to get at the mega-corporation making gi-normous fat profits that is Microsoft (henceforth MS).
I'm also using open-source software to write this blog – OpenOffice.org. And to post to Blogger I use an open-source browser Seamonkey.
There are other issues that make me a fan open-source software ...
In “Third” World countries, such as ours, price and reliability issues are expensive. A ministry, NGO or private user ...
- cannot afford legal copies of MS Office or MS Windows
- cannot afford support contracts
- cannot afford the dial-up Internet time to download latest and frequent security patches for MS products
- cannot afford the anti-virus software
- cannot afford the dial-up Internet time to download the updates to these products.
Many MS products are now requiring you to “authenticate” it over the Internet or by phone/fax – if you don't, it will stop working after a fixed period of time. All very well to stop piracy but ... expensive.
Why did piracy start? Because we cannot afford the original.
Many countries are now promoting the use of open-source software - Brazil, India etc. Certainly, it is a powerful tool in the push to promote Internet connectivity and hence access to information in poor (and not so poor) communities.
P.S. Just added a Creative Commons license to this blog. See the bottom of the page.
Treatment Update
Kezia was meant to start the second (reconsolidation) part of Delayed Intensification 1 (the fourth phase) yesterday. This involves an intravenous dose of cyclophosphamide which itself is particularly nasty. To counteract potential side-effects, especially damage to the kidneys, the child has to have a dextrose/saline drip for 30 minutes beforehand and 3.5 hours afterwards, although the administration of the drug itself only takes 20-30 minutes. This makes a very long day.
However, her neutrophil count has not recovered to >0.75 (x 109/L) so the start of reconsolidation has been postponed a week.
Tuesday, December 12, 2006
Trials, Treatments and Consultants - some sound advice
Yesterday I wrote about a trial of the Augmented BFM phase of treatment which is the second stage of Regimen C.
Through NHS Blog Doctor I came across Christian and Colin Jago's blog auspiciousdragon.net (link on right). Christian has cancer and gives some very sound advice on dealing with it which deserves as wide an audience as possible. In this context I would like to quote some of it.
“The first thing you learn is that the medical profession does not know exactly how YOUR cancer will affect YOU. I happen to believe that conventional medicine represents by far the best approach to seeking treatment ... However, it's not magic. There are so many sorts of cancer and so many complicating factors. Research seems to go something like (1) here is a theoretical approach which might work (2) here is a drug or procedure which might be able to be used to exploit that theoretical approach (3) the clinical trials show that use of that drug or treatment apparently helped a statistically significant proportion of patients (or not). But even if it did, that's not to say, of course, that it will help you, or, more subtly, that if you get better or don't get worse whilst taking/undergoing whatever-it-is, that there is any necessary causative link ...Your consultant can talk in statistical terms but not, even with the best experience and training and diagnostic skills, be SURE that you belong to the statistical group he or she has in mind.”
So however optimistic the stats sound, it is wise to treat your own case cautiously and remember that you might be part of the 10% or 20% or whatever on which the treatment does not work. That being said trials are worthwhile participating in, otherwise there would never be any improvements in treatments.
Christian also has wise words about your relationship with your consultant ...
“For me, the upshot is that it’s OK to challenge your consultant’s view by doing your own research and asking questions. However, I wouldn’t go overboard on the challenge (as opposed to research) part in the first instance - your consultant has after all spent years training and (let’s hope) thinking. If you are unreasonable or shrill he or she will just end up marking you down as Awkward Patient and stop listening ... If you really have good reason to believe that your consultant is just plain down-right incompetent to deal with your problem (unlikely but possible) there are also now places where you can get second opinions on the web, although I have not tried any of them.
Accepting or declining treatment is a slightly different issue because it’s based on your own priorities and view of quality of life and so on, not just medical issues. Any consultant who gets angry with you for politely questioning his or her proposed treatment regime deserves a kick up the arse and a complaint to the hospital or the BMA.
If you do want to delve into the detail, it’s a good idea to take someone with you to your consultant’s appointments. Apart from providing emotional support, they can keep track of the questions and answers with you so you don’t forget or miss things. Tell them in advance you want them to help in this way, preferably.
An important corollary is that it’s also OK to leave it to your consultant. I’ve found that highly intelligent analytical people, imagining themselves in the position of a newly-diagnosed cancer patient, tend to assume that they would feel comforted by doing a lot of research themselves - by analogy with being put in some other life-changing frightening position, like say being accused of a crime of which you believe you are innocent. However, the difference is that you are ill. You might feel too ill to summon up the energy for your normal fact-finding, initiative-taking, driven approach. You might feel that the likelihood of finding a magic answer is small enough not to warrant the time taken away from other activities, if you think you don’t have much time.This is a perfectly rational approach and don’t let the “have you seen the article in the Sunday papers about” brigade deflect you from it. You have a right but no duty to second-guess your consultant.
The other corollary of the medical profession’s limited understanding of cancer is that you need to try to get used to living with uncertainty. The more you can do this, the more at peace you can feel.”
I think this is pretty sound advice – we have been very lucky with our consultant J. who I think would pretty much agree with Christian's opinions.
Taking someone with you to appointments is also a sound idea. Equally, it's a good idea to make a written note of anything you want to ask (so you don't forget) and make notes of any seemingly important information in his or her answers. These may lead onto further questions at a later appointment after you have had time to reflect on them. J. has been excellent responding to my emails.
I totally agree with Christian as well about research – but from a carer's point of view. Nanda being on-hand deals with the day-to-day practicalities and anxieties of Kezia's treatment, and taking care of the normal duties of bringing up two children.
Furthermore, she is currently hindered by linguistic, educational and cultural factors – linguistic because she doesn't speak English (and beyond survival it's not on her list of priorities right now, but hopefully this will change over time and, thankfully, the NHS provides interpreters), educational because she only completed eight years of education (we do live in the “Third” World) and culturally because the medical culture here dictates that you kowtow/touch-your-forelock to the medical profession and don't ask questions.
Me, on the other hand, have little more to do than earn the money to support us all, write this blog and do the research! I don't have the limitations that Nanda has – or, perhaps I should say to the same extent or in the same way. I am dealing with new terminology both scientific and jargonistic, I was hopeless at science at school and, when I was a kid, the family GP was definitely a “Dr.” So when Nanda has queries, she does sometimes get me to ask J., but her queries tend to be of a practical nature (the Hickman Line, a perceived side-effect) whilst I ask him “esoteric” shit about MRD, BFM etc. Given our situation, it's probably an ok division of labour.
A long entry – hope it's not been too boring! Please visit Christian and Colin's website (linked to on right) – it's far more than cancer – cookery, natural history and more. I've also put up a link to Cass' Cancergiggles which is also very inspirational!
As Andy inspired me to say when I started this, I should go off-topic!
Monday, December 11, 2006
The Next Four Months - Part 2
At the end of the first induction phase of treatment, Kezia's hair finally began to fall out. She'd resisted so long! Such a shame – her hair was so beautiful, a crazy, wild mix of black mum, white dad. Losing your hair is a predictable side-effect of the chemotherapy. When chemotherapy stops, the hair will grow back – let's hope it grows back as wild and crazy!
She now started the second phase of treatment of Regimen C - what is called “Augmented BFM Consolidation”. First off, the rest of her hair fell out!
Augmented BFM Consolidation contrasts with the standard BFM Consolidation which is used in Regimen B (but not in Regimen A).
Two big differences – standard BFM doesn't use the drug Vincristine which is administered four times in the Augmented BFM or the Asparaginase administered twice. Secondly, there is a 2-3 week interval of administration of major chemotherapy drugs (Mecapturine – 6-MP, and Cytosine arabinoside – Ara-C) in the middle of the Augmented BFM phase.
Recently found an interesting paper in the Journal of Clinical Oncology comparing standard BFM and Augmented BFM treatments for Slow Early Responders (SERs). One of the results was that 90.7% of SERs with T-cell ALL had a 4 year Event Free Survival (EFS i.e. no relapse) rate.
This obviously gives rise to cautious optimism. However, the end of our nightmare is so far down the line from here that I rarely think of a life without leukaemia – in fact, we will probably always live with it even with a four year EFS, what about a 10 year EFS?
During the entire treatment, regardless of regime, your child will receive an antibiotic, called Co-trimoxacole, at home on Saturdays and Sundays. As your child's white blood count is low and s/he has little protection against infection, this is thus a precautionary protection. It's euphemistically known as the “weekend medicine”.
Friday, December 8, 2006
The Next Four Months - Part 1
The next four months are still painful to talk about. And I'm not sure how to talk about it ...
I came back here and Nanda had yet to receive a 2 year extension to her 6 month visa. I couldn't apply for a 2 year visa for Jaime until she had the extension – I've explained all this in the previous post on Immigration.
Nanda's extension came through about the end of July and I immediately applied for Jaime's visa. But it took time ...
In the mean time, Nanda beat up on me constantly – as M. said she would!
The first crisis had happened before I came back – H. had been carrying Jaime on his bicycle and Jaime had caught his flip-flop in the back wheel and over they came! Jaime needed two stitches to his forehead (the very small scar is there 'til today and, yes, I know, carrying a second person like this is dangerous but I live here in Africa ... three/four people on a motorcycle is common!). Nanda and I only learned about this after I came back ... and she didn't learn through me!
The second crisis was that first photo I took of Jaime which I related earlier.
At first Nanda wanted Jaime to spend the weekends at his uncle's (her brother A.). After three weekends he didn't want to. He played lots with our neighbours' kids and considered them his community. There aren't many neighbours' kids around where A. lives, so he was obliged to play all day with his two years younger cousin. I also didn't want him to – especially when I gathered his natural father (several previous and current partners with numerous children – fortunately, his name is not on the birth certificate) had visited him there. As he's never shown any real interest in Jaime, both Nanda and I feel he should keep away. And I didn't want him to know anything at all about our future plans – to turn up at the airport on the day of departure and make problems!
The next event was Jaime's birthday on the 30th July – 7 years old! We had a small party with a cake, food etc. Sang “Happy Birthday” and blew the candles out.
Photos were, of course, sent to Nanda and Kezia, and this time I got no complaints!
In the meantime Jaime moved into my bedroom, started school again and we settled into a steady rhythm. We'd get up, get washed, H. would arrive and prepare his breakfast, I would go to work, Jaime would have lunch and then go to school, I'd return from work, H. would go home, I would prepare Jaime's bath, he'd come home at 17:20, take his bath, eat dinner whilst I had a shower, watch children's TV until 19:00 and then it was bed and my TV.
I enjoyed the rhythm, the discipline of childcare – it did me good, gave me responsibility and made me (somewhat?) responsible.
I would phone Nanda or she would phone me ... and she'd harangue me constantly “where's Jaime, how's Jaime, when's Jaime coming ...?”. I couldn't run any faster than the seemingly slow bureaucracy of the IND. I would ask about Kezia and receive the response “where's Jaime, how's Jaime, when's Jaime coming ...?”.
I know it was hell for Nanda – she was having to cope with a strange country, a language she didn't speak, the hospital etc etc.
To be continued.

Wednesday, December 6, 2006
UKALL 2003 - Regimen Schedules
I'll now try and explain the differences between the three regimens (A, B and C). They are basically the same length of time – 2 years for girls and 3 years for boys (yup, being a girl gives you an advantage!).
Regimen A
Weeks 1-5 Induction
Weeks 6-8 Consolidation/Central Nervous System Stage II (stage I was part of the Induction)
Weeks 9-16 Interim Maintenance no.1.
Weeks 17-23 Delayed Intensification no.1
Weeks 24-31 Interim Maintenance no.2
Weeks 32-38 Delayed Intensification no.2
Weeks 39-50 Maintenance Cycle no.1
Weeks 51 ...
These maintenance cycles then just repeat themselves until the end of the treatment - 112 weeks for girls and 164 weeks for boys.
Regimen B
Weeks 1-5 Induction
Weeks 6-10 Standard BFM Consolidation – (BFM stands for Berlin-Frankfurt-Munster - cities in Germany where they worked this stage out),
Weeks 11-18 Interim Maintenance no. 1
Weeks 19-25 Delayed Intensification no. 1
Weeks 26-33 Interim Maintenance no. 2
Weeks 34-40 Delayed Intensification no. 2
Weeks 41-52 Maintenance Cycle no.1
Weeks 53 ...
These maintenance cycles then just repeat themselves until the end of the treatment - 114 weeks for girls and 166 weeks for boys.
Regimen C
Weeks 1-5 Induction
Weeks 6-14 Augmented BFM Consolidation – (BFM stands for Berlin-Frankfurt-Munster - cities in Germany where they worked this stage out)
Weeks 15-22 Escalating Capizzi no.1
Weeks 23-30 Delayed Intensification no.1
Weeks 31–38 Escalating Cappizzi no.2
Weeks 39-46 Delayed Intensification no.2
Weeks 47-58 Maintenance Cycle no.1
Weeks 58 ...
These maintenance cycles then just repeat themselves until the end of the treatment - 118 weeks for girls and 170 weeks for boys.
There may be delays due to, for example, an infection (somehing that will almost certainly happen as your child's white blood count is very low) or the levels of neutrophils are too low to start a certain medication and you have to wait unil they have recovered to a certain level.
I wanted to do a pretty graphic or spreadsheet to show all this but my blogger skills are not up to it yet
From here on in, I think I'll only specifically be discussing Regimen C – as I'm not in a position to specifically discuss the ins/outs of the other regimens as they pertain to your child. Regimen CKezia, as I've said, is on Regimen C.
I will talk more about treatment, protocol etc but in the next post I'll try and focus on the story and post a photo or two!
What I will say is that the doctors will take your child off regimen/protocol if there is any doubt that it's not working, if any test reports are not as expected, if your child shows any bad reactions to medication. They will then “hack” it – to the best of their considerable knowledge.
Although many children are showing regular or standard patterns of ALL and responding to the standard treatments outlined above (and, thank your deity, until now, Kezia is), some will not, and as we know so little about such cases, the doctors have to respond to each new development as best they can.
H. is a case in point, and my colleague M.'s wife as well (although we're not talking ALL in her case).
Tuesday, December 5, 2006
Jaime
UKALL 2003 - the Trial
I talked briefly about the objectives of the UKALL 2003 trial in an earlier post but will go a bit deeper into it here.
Initial allocation to a treatment regimen is based on the patient's age, initial white blood count and response to treatment at Days 8 and 15.
Minimum Residual Disease is a very fine genetic measurement tool to quantify remaining leukaemic cells in the bone marrow and is much more accurate than the traditional methods of counting leukaemic cells under a microscope.
The aim of this part of the trial is to see whether the intensity of treatment can be reduced for children with varying levels of MRD without effecting their chances of suffering a later relapse (or Event Free Survival – EFS - as it is known). The advantages of this is that many of the drugs used to treat leukaemia are highly toxic leading to a range of less and more serious side-effects. If fewer drugs can be administered, will this effect the outcome of the treatment?
At the end of the first block of treatment a measurement of Minimum Residual Disease (MRD) is taken. Children (whose WBC is satisfactory, fulfill age criteria, have had no complications etc) will be assigned randomly to Regimens A or B if their MRD count is considered low, or Regimens B or C if their MRD count is high.
There are really no advantages nor disadvantages to participating in the trial – its swings and roundabouts.
In Kezia's case her white blood counts were still too high to participate in this part of the trial – she was automatically assigned to Regimen C.
Another part of the trial is to evaluate a new form of the chemotherapy drug Asparaginase. Previously, it was necessary to have more frequent injections of Asparaginase. By pegalating the drug, it is released far more slowly into the bloodstream thus necessitating fewer injections. Pegalating a drug involves adding a molecule of polyethelene glycol to it. The study is basically looking at how pegalated asparaginase behaves – its release rates, how long it survives in the blood. It goes under the trade-name Oncaspar which you will also hear being used.
The final component of the trial is to assess Quality of Life aspects of leukaemia and leukaemia treatment for both the child and its parents. This is done through administering a short questionnaire at five time points during the treatment.
Monday, December 4, 2006
A New Colleague
So I arrive back at 2 am after a gruelling trip.
Nanda super-filled the suitcase with presents for back home. There are lots of steps with no escalators or lifts (from London Euston underground to London Kings X underground. Then there are even more stairs from London Paddington underground to Paddington mainline railway station). I suffered from muscle-strain pain for weeks!
I got to Lisbon at around 20:30, the onward flight due at 23:50. ... and waited and waited and waited ...
They took us to the plane and from the plane – twice! Eventually, at 3.00 am, they taxied us to a hotel downtown Lisbon. TAP (Portuguese Airlines) is euphemistically known as “Take Another Plane” - but we can't!
Finally, at around 17:00 on the Sunday we departed, arriving here in the early hours. As I was so fed up with all this, no longer had any patience to deal with this and as I know the immigration people, I just handed in my passport into them, and I'll pick it up later in the week.
Nanda's brother was there to meet me and took me home to see H., his wife K., their daughter J. and, of course, Jaime. H., who works for us has been living here for the last few weeks with his family looking after the house and Jaime.
First big mistake – I take a photo of Jaime – he's dirty, having come back from playing with neighbours' kids but happy. I forward this to Nanda, thinking she'd like to see Jaime fit and healthy - but she goes ballistic!
Off to work on Monday and meet a new colleague M. M.'s wife is from the Philippines and is on a second round of cancer treatment. I don't know the medical details but she's on relapse right now and it has spread from one organ to another.(This week it's confirmed it's gone to her bone). Prognosis is not good.
We get on well – lots of talk about cancer, lots of talk about emotional things – he tells me that Nanda will beat up on me for at least a year.
Both of us far away from our loved and sick ones, we continue to exchange progress reports, blood and biopsy reports etc etc.
He's applied for a job with another branch of our employer (giving more money, of course) and if he gets it and moves away from here, I'll really miss him. So I don't want him to get it!
Thanks M.
Friday, December 1, 2006
Expatriates
London has a small community and there are a few scattered elsewhere around the country.
The town in which we live in the UK has a population of 205,000 and a small African community – enough to establish a small NGO that runs a community centre with a food shop next door. My brother had been trying to get in touch with them but with little success. So when I took Jaime over in November, I dragged Nanda and Kezia off to see what they did.
We were met at the reception by a Gabonese man who explained a little of their activities. He then said oh and the woman working in the shop next door speaks the same language as Nanda, I think she's from ..., I'll call her over. Turns out that she's right from our own country! An amazing coincidence!
So the next 2 hours are spent talking and talking and talking ...
A real morale booster for Nanda - I hope she has stayed in touch.
Our Cousin
Someone who has been incredibly supportive to us, although somewhat at a distance, has been Nanda's cousin SL.
I met SL here many many years ago – early '90s I think – when she'd just started at the BBC and was accompanying another (Anglo) BBC journalist here to cover something or other.
We became firm friends over time, especially as she was/is a great friend of my ex-partner.
When I met Nanda, they didn't even know (of) each other. Only after talking to Nanda's father, did I discover that he was SL's father's nephew (so strictly speaking SL and Nanda's father are first cousins). Everyone here seems to be related somehow or other!
SL continues to work for the BBC, has gained a B.A., M.A. and UK nationality.
She hopes to come back here and is building a house here ... but I fear will never find gainful employment here. She has absorbed the journalistic standards of the BBC. She came back briefly in the late '90s and started an interview program on national TV asking hard-hitting questions of our politicians – and they didn't like it. The politicos/ruling-class put the pressure on, the program was axed and she returned to London.
Although we have a multi-party democracy since 1992 (semi-functioning but very successful in African terms – another post), and officially censorship is not permitted, journalistic self-censorship is common. SL would not accept this.
She's also a published poet – though I don't think anything has been translated into English yet.
SL lives in London – about 350 miles from us. But she has visited and phones regularly. She has seen us through some emotional crises, talking to and calming down Nanda when I couldn't.
Thank you SL – you supported me before Nanda and you support us now.
Thursday, November 30, 2006
Good News
There's only one flight a week direct to Europe so you can imagine that at this time of year reservations are a bit difficult. At first there was no place on the return leg but my friend L. pulled it off! Many thanks (again!).
Wednesday, November 29, 2006
Going Home
At the beginning of the fifth week, we were allowed to go home. Not back here! But to the rented house. Now Kezia was to start the next stage of treatment as an out-patient. The hospital would provide transport and an interpreter for Nanda.
 The new home
The new homeWhat a relief to get home. The coming days were filled with orienting Nanda – local shops, down town, money, buses, bank, switching on the central heating, the gas fire (we don't have such things back here!), paying the rent, the bills.
A brief respite before we started the second stage of treatment - “Augmented BFM Consolidation”. Particularly intensive – but I'll talk about that in a medical post.
We also had visits from our social worker T., the Macmillan Community Nurse from the hospital A., and the local health worker C. C. has helped us out a lot in the last few months.
Immigration again – “No Recourse to Public Funds” on Nanda's new two year visa (and later Jaime's). I'm probably putting us at lots at risk with the immigration authorities here by discussing such things on this blog.
So let's hope no IND officials or racists read this ...
So we registered Nanda and Kezia with the local NHS doctor - General Practitioner/GP in the UK (our family doctor). At the same time the hospital (RMCH) advised the GP not to treat Kezia – everything to do with Kezia must go with the hospital - obvious.
Recently there was an item on the BBC news website that GPs (through the British Medical Council) refused to be policemen for the Immigration and Nationality Directorate (IND) of the Home Office for illegal or abusing immigrants.
On the IND website it advises what “No Recourse to Public Funds” means, seemingly, the NHS, Child Benefit (it's for a UK child, not a foreign mother for godssake) etc etc – but not education. So we have been able to put Jaime in the local primary school. If doctors are refusing to monitor immigration status, can you imagine teachers ...!
I must say, though, that the FCO through the Embassy and the IND have bent-over-backwards to help us. I don't blame them in the immigration requirements – they are, after all, following the regulations, laws and Acts of Parliament which they are duty/job-bound to follow.
Meanwhile, I needed to come back here. My job is here, our house is here, Nanda wants to come back here, I want to stay here ... and I have to earn some money to keep them in the UK.
Especially, as an IND requirement is that they (Nanda and Jaime – Kezia is a Brit) don't want to stay in the UK indefinitely and we can only prove that by me, a UK national, saying I don't want to stay in the UK indefinitely. Kafka?
So on Friday 7 July I set off back here.
Kezia, Baby and the Menagerie
Monday, November 27, 2006
UKALL 2003 - Regimens A, B and C
The UKALL 2003 trial initially chooses your child's treatment regimen based on a series of diagnostic tools - prognosis factors based on previous experience and lab tests. Thus ... I will try to reinvent the wheel as I promised not to do previously.
If your child is under one year old, s/he will go onto another protocol trial.
If your child's ALL is effecting the White Blood B-cells (see the post on Haematology), s/he will follow a different protocol developed by the UK Childhood Cancer Study Group (sorry – I don't know any details right now). UKALL 2003 is only involved with T-cell ALL.
If the child has any of various genetic abnormalities which have been shown to put the child at a higher risk of later relapse, then s/he will automatically be put on Regimen C.
If your child is older than 10 years old, then s/he will automatically be put on Regimen B.
If your child has an initial White Blood Count (i.e. mostly malformed T-cells) greater then 50 (x 109 per litre), then s/he will go on Regimen B.
Kezia “passed” all the above (phew!) except the last one. So she went on Regimen B. I was confused at first between Regimens B and C – don't worry, in the first stage of treatment Regimens B and C are the same. They differ in later stages of treatment.
They then look at the number of lymphoblasts in your child's bone marrow at Days 8, 15 and 28 of the initial treatment.
If at Day 8 and the child is on Regimen B and the blood-producing cells of the bone marrow show more than 25% lymphoblasts, then s/he is automatically transferred to Regimen C. S/he is also thus classified a Slow Early Responder (SER). This was the case with Kezia (and by the way H.).
If your child is on Regimen A and there are more than 25% lynmphoblasts at Day 15, then s/he will go onto Regimen C.
If your child is on Regimens A or B and has less than 25% lymphoblasts at Days 8 or 15, then s/he will stay on the same Regimen (course of treatment).
If your child is older than 16 years, s/he will continue on Regimen B regardless of the Bone Marrow results.
The next bone marrow test is at Day 28 – the end of the Induction phase. If your child has already been assigned to Regimen C, this will not make any difference.
However, if your child is on either Regimens A or B, then the 28 day count can decide the future course of treatment. If your child still has between 5% and 25%, s/he will go onto the Regimen C treatment. More than 25% s/he will stop being part of the UKALL2003 trial and will be treated under another protocol.
Less than 5% of lymphoblasts, your child will be allocated randomly to Regimens A or B.
This is really one of the objectives of the trial. As I said before, Regimen A is the least intensive/aggressive and Regimen C is the most intensive/aggressive. The drugs for killing the leukaemia attack both good and bad cells. They want to see if a low-level of leukaemia, needs less amounts of drugs to kill the disease. They cannot take too many risks with our treatment, so only children with less than 25% at days 8/15 and less than 5% at Day 28 will really go on to experiment between Regimens A (less aggressive) and B (more aggressive).
I'll about the differences between the regimens in a later post.
Wednesday, November 22, 2006
Shingles
Shingles is caused by the same virus as chickenpox (varicella-zoster). Whilst children get chickenpox, adults get shingles. Immuno-depressed people, such as those with leukaemia, are particularly prone to infections such as this.
Will be thinking of you.
Tuesday, November 21, 2006
Medical Stuff - Part 2: UKALL 2003
I'll go into greater details about the objectives of the trial in a later post but basically it aims to evaluate whether different treatment regimes will have a effect on full recovery/later relapse rates.
The prognosis for successful treatment is now fairly good – around 80-85% of young children will not suffer a later relapse. There are a number of factors that can influence successful outcome. Being so young and being female make Kezia's prognosis better. The gender difference means that boys receive 170 weeks of treatment and girls 118 weeks.
There are three regimes – A, B and C. A being the least intense treatment regime and C being the most intense. The regime a child follows depends on a lymphoblast count in the bone marrow on days 8 and 15 of the first stage of treatment + some other factors, such as whether lymphocyte B-cells or T-cells are affected (B-cells s/he comes off the trial and follow different treatment – sorry, but I know nothing about it).
Kezia had a bone marrow lymphoblast count of > 50 (x 109/L) when she was admitted so she was automatically assigned to Regimen B. As her count was still greater than 25% at Day 8 she was then assigned to Regime C. What is called a Slow Early Responder (you got it – SER) as opposed to a RER (have a guess! ... Rapid Early Responder)
Her initial very high WBC/malformed lymphocyte counts indicated that she'd probably had leukaemia for a few months. We'd noticed symptoms but neither the doctors here nor ourselves could interpret them. We had noticed some unwillingness to walk, in March she fell down the three steps to our veranda, twisted her ankle, leading to even more unwillingness to walk – we didn't know that an effect of leukaemia was pain in the soles of the feet.
Although her lymphoblast count at Day 28 showed full remission had occurred, the trial protocol specifies that the treatment regime is decided based on the Days 8 or 15 lymphoblast count.
I won't go into all the variables that decide which Regime your child will follow –I would be reinventing the wheel as a square - please consult the protocol documents on the UKALL 2003 website and speak with your doctor.
However, I will say that the massive increase in recovery and survival rates over the last 30-40 years has been due to children participating in such trials and that we also should participate for the sake of future sufferers of ALL and in the hope that their opportunity is even greater than that of our own children.
Payback.
Photos
Monday, November 20, 2006
Medical Stuff - Part 1: Haematology
Ok, I'll take the plunge and try to explain a bit about what Acute Lymphoblastic Leukaemia is and how Kezia is being treated. If I get anything wrong, and any of our readers are in the medical profession, please correct me through the Comments or by email.
First we need to take a look at blood. The study of blood is haematology. Haematologists are doctors who know a lot about blood. If you don't understand a bit about blood, you won't understand much about leukaemia.
Blood cells can be divided into three types: red (RBC), white (WBC and also known as leucocytes) and platelets (PLT). You'll see these abbreviations on lab reports so I'll start using them now.
When you whizz blood around at very high speed in a centrifuge, it separates out into these three types: white cells are white, red cells are red and platelets are a kind of bilious yellow.
Red cells are important for carrying oxygen and other nutritious things round your body. White cells defend your body against all the millions of things that would like to attack and eat you. Platelets are there to clot your blood if you cut yourself – those nasty scabs form because of platelets – if you didn't have them, you'd bleed until there was no blood left at all - which means you're dead.
The important ones as far as leukaemia goes are the white cells, and, sod's law, there's a bunch of different types which we need to get to grips with.
- Neutrophils (MNEUT): these constitute around 65% of the WBCs. They defend you against bacterial infections and are the first ones to respond to an attack. Kind of like suicide bombers in that they die during the attack and turn into pus.
- Eosinophils (MEOS): these constitute around 4% of the WBCs and defend against parasitic infections.
- Basophils (MBASO): less than 1% of the WBCs. These are responsible for responses to allergies and release histamines causing inflammation.
- Lymphocytes (MLYMPH): around 25% of WBCs. Divided into further sub-types.
- B-cells - these make antibodies that bind to the attackers enabling their destruction. The arms factories.
- T-cells - CD4+ (helper) cells coordinate the immune response – the generals telling the different troops where to go. CD8+ (cytotoxic) cells are the SAS of WBCs that kill virus infected cells. Natural Killers are the MI6 of WBCs. They can kill infected cells that are displaying a signal to the other troops not to kill them (hello I'm friendly! e.g. cancer cells).
- Monocytes (MMONO): 6% of WBCs. These are similar to our MNEUTs but get to live a bit longer.
All of these are produced in the bone marrow. And they all derive from Hemopoietic Stem Cells (HSCs), also known as Hemocytoblasts. These cells split and form precursors of all of the above as well as the precursors of RBCs and platelets. The immediate precursors are known as blasts which then develop into the -cytes above before being thrown out into the blood to do their work.
 In Acute Lymphoblastic Leukaemia something goes wrong with the HSCs. They start producing more and more lymphoblasts which never grow up into lymphocytes. The lymphoblasts take over all the space in the bone marrow allocated to the the other types of blasts – red, white and platelets. This gives rise to low RBC levels (anaemia) and low platelet counts (danger of bleeding).
In Acute Lymphoblastic Leukaemia something goes wrong with the HSCs. They start producing more and more lymphoblasts which never grow up into lymphocytes. The lymphoblasts take over all the space in the bone marrow allocated to the the other types of blasts – red, white and platelets. This gives rise to low RBC levels (anaemia) and low platelet counts (danger of bleeding).
They also head out into the blood. As they have not matured into lymphocytes, they can't fight the attackers as they should. Hence people with ALL are prone to infections.
Initial diagnosis is by a blood test - positive results show a large number of lymphoblasts. This is then confirmed by a bone marrow sample which, if positive, will also show a large number of lymphoblasts.
Other clinical signs are an enlarged spleen (WBCs accumulate here), anaemia (lack of RBCs) and a reduced platelet count.
Friday, November 17, 2006
The First Four Weeks - Part 3
While all this was going on at the hospital, I also had a lot to see to on the “outside”.
Kezia's passport, Nanda's visa extension, a new driving license (I only had the old-style green one) and, above all, finding a house to rent.
We preferably wanted something near to my brother and sister-in-law. My brother got the local paper on Saturday – there was a fully-furnished back-to-back terrace 30 seconds round the corner! We went and peered through the windows – looked ideal! Monday was a bank holiday so first thing Tuesday morning I rang the estate agency and said I wanted it even without a viewing! Arranged a viewing anyway and gave our sob-story. There were other interested parties but we got it!
It's ideal – down a short alley off the main road. A late 19th century terrace of five houses with a small garden directly in front of the house. Great for kids with no traffic to worry about. Fully-furnished, as I said, and the previous occupants had even left a hi-fi which was not on the house inventory!
Being tucked away as it is, the only disadvantage is that no taxi driver has ever heard of it! We have to give the address of the back-to-back behind us on the main road.
After signing the contract, I then had to set up the electricity, gas, telephone, TV license and council tax. Blimey everything has changed from when I last lived in the UK – now you can do it all over the phone and pay at the local shop!
One of my sister-in-law's sons donated a television, the other a mobile phone. Necessities such as bedding, pots and pans etc had to be bought.
Meanwhile at the hospital we were being prepared to leave and for Kezia to continue treatment as an out-patient. The major preparation was to train us in the administration of medication via the Hickman Line. Two training sessions and we were deemed competent. It really needs two people – one to clean the line, administer the medication etc and one to hold Kezia and check the first person is doing it all correctly. So when we finally got home, and as I would be coming back here, we trained my brother, sister-in-law and one of her sons on how to do it as well.
Immigration
You may have been wondering why Jaime hasnn't figured much in this so far ...
First, Jaime didn't come with us back in May. I'd booked a ticket for a week, Nanda and Kezia for a month. Little did we know ... We employ a really trustworthy guy (H.) to look after the land (smallholding-size: 60 m x 60 m) around our home and we asked him and his family (wife K. and small daughter J.) to come up and live here, look after Jaime and the house. They did an admirable job! Thanks! As they live with Mum, brother (+ ...), sister (+ ...) in a very small wooden house it's a bit of a holiday for them (although living on my own now concerns everyone – it's a far more “social” society than the UK).
Then, when we discovered it was leukaemia and the length of treatment (c. 2 years for girls, c. 3 years for boys), we had to apply for Nanda to stay longer than the initial six months granted at Heathrow.
Getting a passport for Kezia was not a great problem. Although I am Kezia's registered father, Kezia cannot receive my nationality if I am not legally married to the foreign mother – Margaret Thatcher's bloody 1981 nationality legislation! (If it was the other way round – UK mother, foreign father – no problem). Having discovered this early 2006, we got married on February 4 2006. (As you can gather formal marriage is rather against my personal philosophy!) Fortunately, the 1981 Nationality Act is “retrospective” so even though we married after Kezia was born, she still receives UK nationality through her dad. Now Kezia is the proud owner of British Citizenship and a UK passport! Not that she really cares right now.
Nanda was more complicated ...
The Embassy and the Passport Office had signed off on Kezia being a British Citizen. The Embassy had signed off that Nanda is my wife. However, to extend Nanda beyond 6 months, we needed: translated documents, birth and marriage certificates, bank statements (here and there), statements of income and contract length from my employer, proof of will return to country-of-origin (letter from my employer), letters from our consultant J. and social worker T. etc etc. Took a time but we got it.
On to Jaime ...
The embassy can only grant 6 month visitor's visas. Obviously, we wanted Jaime to get the same as Nanda. So first we had to wait until Nanda's 2 years came through. Then we had to send Jaime's passport and all the same documentation cited above to the embassy (in Angola as you will recall) who then had to send it all to the Immigration and Nationality Directorate in the UK. First difficulty was getting it all to Angola – DHL costs an arm and a leg if you don't have a contract with them. I rang my friend B. who works at the top hotel here to see if they had a DHL contract – no, but hang on a minute. An aunty of an employee, an Angolan judge, was staying at the hotel and returning to Angola tomorrow. I raced down to the hotel and she hand-carried everything to the embassy – I can't remember your name but many thanks!
The return leg was facilitated by JG, our hon British consul and a local businessman, who happened to visit Angola just as the visa came through.
I picked up Jaime's passport on 29 October and we were on the plane to the UK on 5 November!
Took a while and Nanda really didn't understand why it was taking so long when for her and Kezia it only took three days!
Again many thanks to L. at our local travel agency.
And many many thanks to the UK embassy in Angola who have been absolutely amazing throughout this ordeal.
You may wonder why I'm the only member of the family posting – well, Nanda and Jaime don't speak English (yet!) and Kezia's a bit too young to have mastered either the lingiustic or computer skills. If this blog survives, hopefully you will see entries from them in the future.
This weekend I'll try and get some medical info. written. Still can't upload photos. See you on Monday.
Thursday, November 16, 2006
The First Four Weeks - Part 2
The staff at the RMCH are all kindness. Too many people to mention or remember.
But I would like to mention a few. First our consultant, J. He's marvellous. Takes his time to talk to you, explain the illness, the treatment etc. I quite quickly went and bought a couple of medical textbooks on haematology (blood) and oncology (cancers) so I could ask him sensible questions. Obviously, this gave rise to more questions as I tried to get my head around neutrophils, basophils, hematocrit etc etc and their significance in test results. J. takes his time to explain to you, at your level and without being in any way condescending. He really shows sympathy to what you and your child are going through. He has continued to answer my questions from afar. Thanks J. for your patience and kindness.
Secondly, our hospital social worker, T. Again >200% sympathetic. Bits of money here and there which she has arranged have really helped out. The social services at the hospital are contracted out to a NGO called Clic Sergeant (see link on right). They automatically give each new patient ₤200. Since she has found us bits of financial support from various sources. Always ready to listen. And helped out a lot getting letters written to support our immigration/visa issues. Thanks T.
The nursing staff are wonderful. So clearly love kids. Special thanks to H. (hope the pregnancy went well!) and E. You showed special kindness to us. You are allocated to a couple of nurses who meant to give you special attention, kind of mentoring you. Not sure this works too well given they work shifts, take leave etc. Anyway, all the nursing staff are great.
Other parents – we all tend to be a bit wrapped up in our own problems. However, we made special friends with A. and her daughter H. (who I mentioned briefly earlier). H. was admitted about a week or so before us and just before her 16th birthday. Whilst Kezia's treatment has so far all gone according to plan, H. (and obviously her family) has been to hell and back. Every side-effect in the book and more. Medication-induced diabetes, blood clots in her legs, mucosis that has made her saliva green etc etc. Most recently contracted ankle tendons that have required her lower leg to be set in plaster. All this in addition to “normal” side-effects such as tingling feet, hair-loss and mood-swings. You are very very brave! A., you've been a wonderful support – just talking and sharing feelings has helped me so much.
Thanks to all of you! I will never ever hear the National Health Service be knocked again!
Each day would fly by. Bathing Kezia, breakfast, doctors' rounds, meeting J., meeting T., other specialists, taking temperature and blood pressure, treatments (pills, drips, injections), transfusions (blood and platelets), paperwork, interpreting for Nanda, lunch and dinner, laundry, visits from my brother and sister-in-law, phonecalls to/from family, playing with Kezia. And, above all, learning about leukaemia. A steep and rapid learning curve!
Parents are given blood test results but don't have an automatic right to see their child's entire clinical file. I summoned up the courage to ask about this, not wanting to make anyone uncomfortable that I had any doubt whatsoever about the excellence of the treatment Kezia was receiving. After asking the ward sister, I headed off to the Patient Advice and Liaison Service (I think that's what they call it). Apparently, if you want to see your child's file, you have to write a letter to hospital management. You will the be granted permission to see the file under supervision. You can request photocopies but pay for them. Later, I talked to J. about this and he said he'd willingly show me the file if I wanted. My confidence in him, his patience in explaining everything, led me to decide I really didn't need to see it right now.
At first we were allowed to take Kezia out in the hospital grounds. There's a nice garden with a small aviary with parakeets and budgerigars (donated and built in memory of a past African-origin patient) so we'd take Kezia down there. In the third week we were allowed to take Kezia out to the local park where we'd play on the swings and slide.
Kezia has never had a pushchair as back home the almost total lack of pavements and the numerous potholes make them pretty impractical. Well, Kezia has decided she ain't going to start now when it's much more warm and comfortable to be carried in the traditional African way on mum's back! Even after my sister-in-law brought her a beautiful bald black doll with her own pushchair! Kezia was quite happy pushing Baby around but herself – not likely. We managed it a couple of times but she was definitely not keen. The pushchair we have since bought remains the preserve of Kezia's menagerie of stuffed toys! In fact, whenever Kezia is upset, going on mum's back is a sure way to calm her down even to the point of sleep. The hospital staff were amazed.
See this link about African women and pushchairs
For some reason Blogger isn't allowing me to post photos today - will add some to this post when this is resolved.
Part 3 to follow











